Here are some of the questions we are asked most frequently. We hope that you will find this helpful. If you have any questions not included below please get in touch using our contact form, or by emailing contact@forteability.com
A stoma is a surgically made opening on your abdomen where a piece of bowel is brought through to help you pass faeces/urine into a stoma pouch.
Yes, there are three main types:
- Colostomies constructed from the from the large intestine/colon. The output is stool or faeces
- Ileostomies constructed from the small intestine /ileum. The output is stool of faeces.
- Urostomies constructed for drainage of urine
Some stomas are permanent, and some are temporary. A temporary stoma can become permanent.
There is no ‘best’ pouching system (bags). In other words, no product is better than another.
The best pouching system is the one that has been prescribed by a qualified, trained stoma care nurse practitioner after careful assessment of the individual’s stoma.
Yes, all stoma products are disposable. The wear time of the products differ based on the type of stoma, the type of output, the site of the stoma on the patient’s abdomen and the size and shape of the stoma. Your stoma care nurse practitioner will guide you on when to change your products.
One should not wait until the product is leaking in order to change it.
Every individual is unique and the pouching system that they are using will depend on the type of stoma they have, how much they sweat, how active they are, their stool consistency/ urine output etc.
- Closed or daily change pouches for colostomies with firm stool are changed 1 – 2 times per day.
- Drainable pouches wear time can vary from 2- 5 days and sometimes longer (exceeding a 7-day wear time is not recommended)
Always change your pouching system (bags) if:
- There is a burning/itching sensation on the skin around the stoma
- If your pouching system is leaking
- If you are experiencing odour
Something has changed! Your stoma may have changed in size or shape, your abdominal shape may have changed due to weight gain or loss, the output from the stoma may have changed. Please see your stoma care nurse practitioner for a re-assessment of your stoma and peristomal skin. It is extremely rare that the pouching system (bags) are faulty.
Something has changed or the pouching system (bags) that you are using is not the correct prescription for you. Please see your stoma care nurse practitioner for a reassessment of your stoma and a new prescription for your pouching system (bags).
No, your stoma cannot become infected. Your stoma is made from your intestines. The intestine is a “dirty” organ and cannot become infected.
The skin around your stoma can become irritated and inflamed, so it is essential to have a good skin care regime in order to maintain healthy skin. On rare occasions, a peristomal abscess may develop.
Always consult your stoma care nurse if you are experiencing pain and/or you have noticed that something has changed around your stoma or on the skin around the stoma.
- Warm water and roller towel/paper towel/disposable cloth
- Soap that is free from oils, moisturisers, and fragrances
- Wet wipes that are free from oils, moisturisers, and fragrances
- Ensure the that any soap is rinsed off and that the skin is dry before applying your new stoma pouch
The skin directly around your stoma should look like the skin on the rest of your abdomen.

Healthy peristomal skin, photograph: Sr Elizabeth Pellencin
- The skin around your stoma may be coming into contact with stool/urine.
- Is your pouch cut to the correct size (1-2mm bigger than the stoma)?
- Are you emptying your pouch when it is 1/3rd full?
- What is your stool consistency like? If it is very loose and watery, you need to thicken it up with the appropriate diet/ medication. If the stool is very thick and sticky, it might be getting stuck to the pouch and not sliding down towards the bottom (this is called pancaking). Speak to your stomaltherapist about adding a lubricating deodorant to your script.
- Speak to your stomaltherapist for a proper diagnosis and treatment.
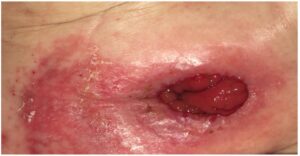
Peristomal excoriation, photograph: Sr Elizabeth Pellencin
- Your stool is too thick and sticky to move down into the pouch.
- Your stoma pouch has no air inside it, causing the stool to collect at the site of the stoma.
- Squirt lubricating deodorant into the bottom of the pouch after you’ve emptied the pouch. Make sure to spread it evenly inside the pouch.
- Pull fresh air into your pouch after emptying it or insert a small ball of paper towel into your stoma pouch to create space for the stool to drop down into the stoma pouch.
- When the stoma pouch and the skin around your stoma is exposed to moisture (water and sweat), you are at risk of developing a fungal infection.
- Ensure you dry your stoma pouch thoroughly after becoming wet.
- Your skin may be exposed to an irritant (soap/ lotion/ perfume).
- Your skin may be coming into contact with stool/ urine.
- Your skin might be dehydrated and dry.
- You may be reacting to one of the stoma appliances or the stoma pouch.
There are many reasons for a stoma pouch to leak, even if you’re applying the stoma pouch exactly the way your stomaltherapist taught you.
- Has your body shape changed in any way (gained/lost weight)?
- Has your stoma changed in shape or size?
- Have you developed a parastomal hernia?
- Has your stool consistency changed?
See your stoma care nurse practitioner for diagnosis and appropriate treatment
- All stoma pouches are waterproof.
- Empty your stoma pouch before entering the water, especially when swimming or bathing.
- Remove your stoma belt before entering the water and replace it once dry.
- Cover the filter of your pouch using the stickers provided by your supplier.
- Your stoma pouch might need changing sooner if you spend a lot of time swimming/ bathing.
- Consider the use of flange extenders.
Once you’re fully recovered and settled at home, returning to the lifestyle you enjoyed before your procedure should be possible. If you have no complications and your healthcare professional has no objection, you can enjoy almost any kind of activity.
- Ballooning occurs when your stoma pouch fills with wind/gas. The wind/gas is produced by you.
- Most stoma pouches have a charcoal filter that neutralises the smell and filters out the gas, but some filters are very slow, or can become blocked.
- Burp your stoma pouch by emptying out the gas from the bottom of the pouch or by gently unclipping the stoma pouch from the baseplate if you have a two-piece system.
- Peppermint tea or peppermint capsules are a great home remedy for when you’re feeling gassy.
- Immediately after your surgery, your anus may continue to expel poop and other fluids that were left inside.
- Some people may have mucus coming out of the rectum/ anus. The bottom part of the bowel no longer has poo passing through, but it still produces mucus.
- The mucus may leak out of the anus, or you may feel the urge to go to the toilet. The mucus is normally clear or white and looks a bit like egg white or glue.
- Sometimes the mucus dries up into a ball inside the rectum and can cause pain.
- Depending on the type of stoma you have, a small amount of poo may pass into the bottom part of the bowel, resulting in a brown discharge.
- If you feel the urge to pass stool, go to the bathroom, sit on the toilet, and gently push out the mucus/ old stool.
- Sometimes a rectal washout is indicated.
Please consult with your stoma care nurse practitioner
It is not recommended to rinse out your stoma pouch as it can affect your wear-time and cause your pouch to leak. Water can affect the odour-proof film inside your stoma pouch, causing the pouch to smell bad. Only clean the tip of the stoma pouch after emptying.
Most ostomates can have intimate relationships the same way they did before ostomy surgery. There may be some hiccups with your sex-drive, depending on the type of surgery you’ve had. If sexual issues arise, speak to your doctor stoma care nurse practitioner for advice.
Some ostomates may have trouble in conceiving a child if they have had extensive surgery. However, most ostomates can have a normal pregnancy and delivery. If you are considering becoming pregnant, speak to your doctor/ stomaltherapist for guidance and advice.
Depending on the cause for your colostomy, you might have to follow a special diet. However, most colostomy patients can eat whatever they want in moderation. If you are unsure, speak to your doctor/ stomaltherapist/ dietician for guidance and advice.
- Ensure that you drink enough fluids throughout the day.
- Ideally your urine should be light yellow in colour. Foul smelling, dark, and cloudy urine are all worrisome signs.
- Keep your urine acidic by drinking a fresh glass of orange juice every day, take 1g of vitamin C daily, or take one cranberry tablet daily
If your healthcare provider has cleared you for travel, there is no reason for you not to.
Planning is very important.
- Make sure you have enough stock with you.
- You are not allowed to keep scissors on your person, so keep a few pre-cut pouches and accessories on you in the event you need to change your pouch while on a flight.
- Your stoma pouch will not explode with the change in air pressure
Ask your stomaltherapist for a travel communication card to avoid questions at customs and/or security checkpoints.
